Abstract
Background: Accurate prediction of survival of newly-diagnosed persons with plasma cell myeloma (PCM) is challenging and better prediction accuracy is needed. A prior analysis of the mSMART3.0 model had a C-statistic of only 0.62 (0.53, 0.71).
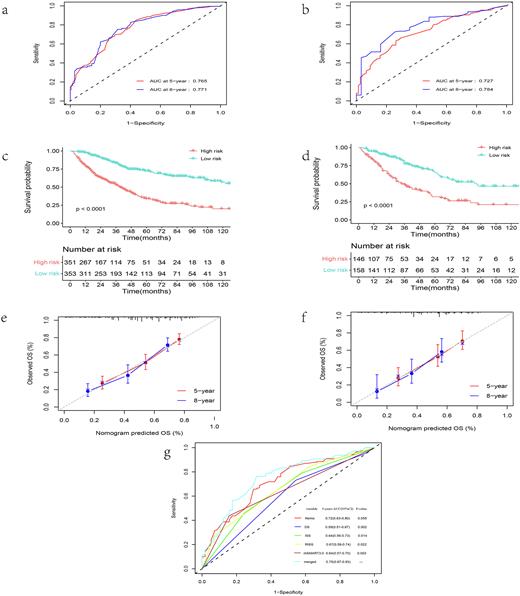
Methods: We interrogated clinical and laboratory co-variates in 1,008 consecutive subjects with newly-diagnosed PCM. Uni- and multi-variable Cox regression were used to identify independent prognostic co-variates to build a baseline nomogram survival model. In 359 subjects whose mSMART3.0 score was known a merged nomogram was constructed to increase survival prediction accuracy. Model performance was assessed by area under the receiver-operator characteristic curve (AUROC), calibration plots, utility and comparison to other survival prediction systems. The cut-off of the risk score was the median risk score of the training cohort.
Results: Subjects were randomly divided into training cohort (n = 704) and validation cohorts (n = 304). A baseline nomogram model using 8 clinical and laboratory co-variates had 5-year survival AUROCs:0.77 (95% Confidence Interval [CI], 0.72, 0.81) and 0.73 (0.66, 0.80) (Figure 1a-b). In the training cohort 5-year survival of subjects in the high-risk cohort 34% (28, 41%] compared with 72% (67, 78%); p < 0.001) in the low-risk cohort(Figure 1c). Similarly significant survival differences were seen in the validation cohort(Figure 1d). The model showed good discrimination and good calibration in the training and validation cohorts (Figure 1e-f). The merged nomogram increased 5-year survival AUROC of from 0.64 (0.57, 0.71) to 0.75 (0.67, 0.83; p = 0.003) in the training set (Figure 1g).
Conclusion: Our model and nomograms improve survival prediction accuracy in newly-diagnosed persons with PCM.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.